March is National Brain Injury Awareness Month. This year, Crosley Law wants to highlight the destructive impact of pituitary dysfunction (PD), which can occur as a part of a traumatic brain injury (TBI). Keep reading to learn more about this commonly overlooked, but life-changing, condition.
What Is Pituitary Dysfunction?
The pituitary gland secretes hormones and is sometimes referred to as “the master gland” because it controls other glands throughout the body. Pituitary dysfunction occurs when either the gland itself or the connection between it and the hypothalamus is damaged. (The hypothalamus is an area of the brain that also regulates hormones and controls bodily functions like hunger, sleep, temperature, and more.) Damage to the pituitary or its connections causes an imbalance in the body’s hormone production.
Because several organs and parts of the brain that regulate hormones are clustered together, damage to this area of the brain during a TBI can have devastating effects.
Common symptoms of a pituitary dysfunction include:
- Fatigue
- Insomnia and disrupted sleep
- Impaired cognition
- Memory loss
- Emotional disturbances
- Weakness
- Weight change
- Sexual dysfunction
Symptoms can develop immediately after a traumatic brain injury or they may manifest weeks, months, or even years later, making it very important to take any head injury seriously. Furthermore, many symptoms of pituitary dysfunction overlap with the symptoms of a TBI, which can make diagnosis difficult.
RELATED ARTICLE: 4 Signs That You May Have an Undiagnosed Traumatic Brain Injury
Why Concussions Should Be Taken Seriously
Research shows that people who suffer from a brain injury are also at a higher risk for experiencing imbalances in hormone production, such as a pituitary dysfunction. The dizziness, headaches, and vomiting that we often associate with concussions are usually the immediate and obvious side effects of a traumatic brain injury (TBI), but they can also indicate pituitary dysfunction. Because these symptoms are associated with traumatic brain injuries, pituitary dysfunction is frequently delayed, or worse, completely missed.
The pituitary gland is located at the base of the brain. During a car crash, fall, or another traumatic incident, the brain can forcefully jolt back and forth within the skull, damaging the brain, its tissue, and connected organs like the pituitary gland.
Since the pituitary gland is among the most vulnerable organs when suffering a brain injury, both concussions (also known as mild TBIs or mTBIs) and moderate-to-severe brain injuries require attention and treatment to prevent escalating pituitary dysfunction.
Recent studies report a significant correlation between traumatic brain injuries and pituitary dysfunction. According to a 2015 article from the journal Neuropsychiatric Disease and Treatment, 15 to 20 percent of patients with traumatic brain injuries develop chronic pituitary issues. More broadly, “neuroendocrine dysfunction” (a technical term for a wide variety of hormone production imbalances) may occur in as many as 42% of mTBI victims.
Similarly, a 2019 article in the research journal Pituitary found that up to 46.6% of traumatic brain injuries involve pituitary dysfunction. The study also notes that human growth hormone (HGH) production is the most frequently reported issue. HGH helps the human body develop healthy bone, muscle mass, and assists with normal sexual function. While this study focuses on sports-related TBIs, it’s likely that PD is just as common in other situations.
It’s tempting to think that TBIs aren’t very common, but everyday events like road accidents, falls, and sports-related injuries rank among the leading causes of traumatic brain injury. This means your risk of suffering a traumatic brain injury is likely higher than you think. In fact, according to the Centers for Disease Control and Prevention (CDC), TBIs lead to approximately 2.8 million emergency department visits, hospitalizations, and deaths every year in the United States.
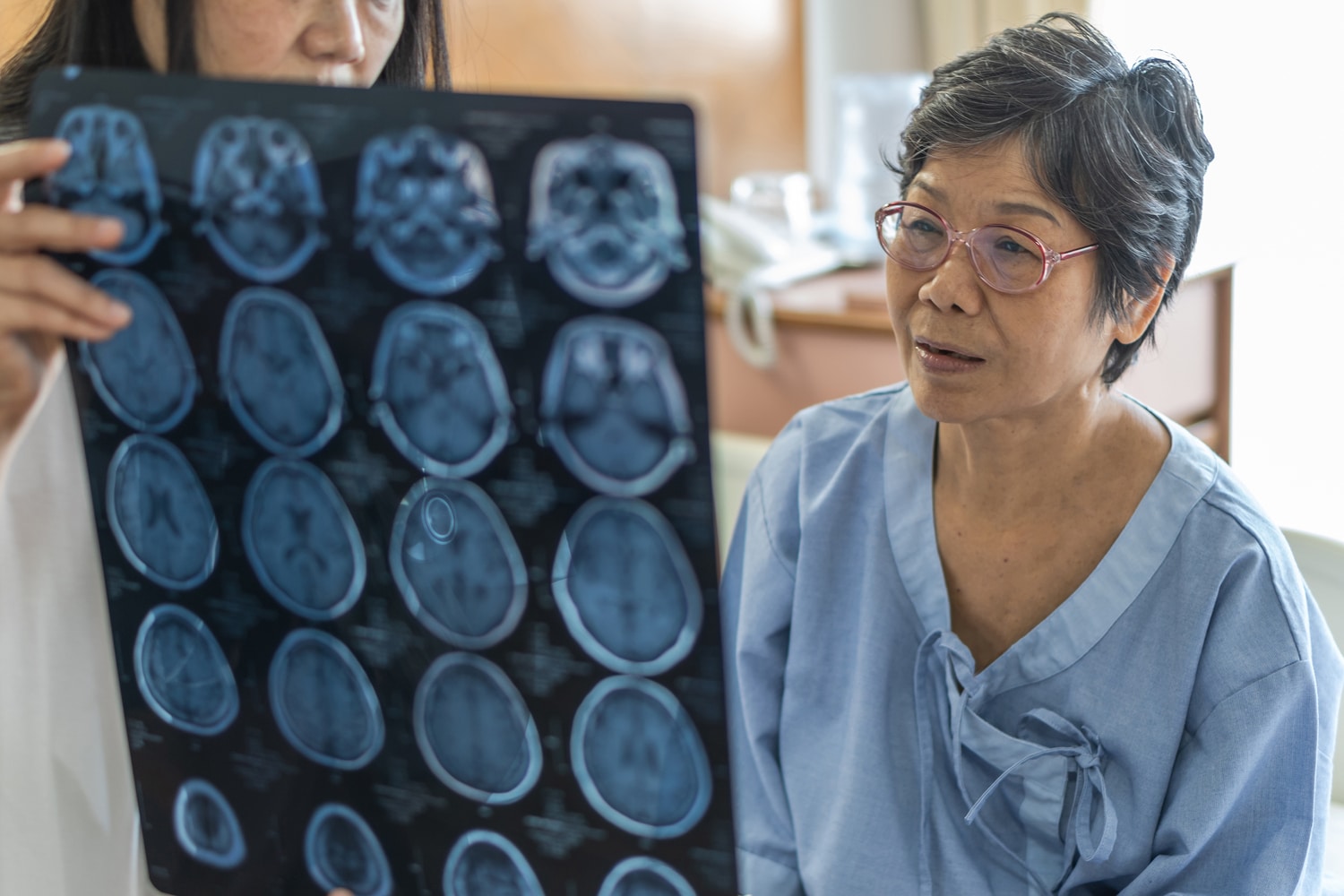
Ask Your Doctor About Screening for Pituitary Dysfunction
If you have suffered a brain injury, you should speak to your doctor about screening for pituitary dysfunction. There are a variety of factors that doctors can take into consideration when determining whether the risk of a pituitary dysfunction is significant for a specific patient. The best way to ensure that you or a loved one is not at risk after a TBI is to speak to your doctor about screening and undergo an evaluation from a qualified medical professional.
You should also consult with an experienced TBI lawyer. At Crosley Law, we are pioneering the way that traumatic brain injury cases are researched and litigated. Our team uses cutting-edge technology, works with some of the leading experts in neuroscience, and understands how deeply a TBI and associated PD can impact your life.
RELATED ARTICLE: Traumatic Brain Injuries: What Victims Need to Know
Crosley Law: Advocating for Traumatic Brain Injury Victims
Crosley Law has a long history of handling traumatic brain injury cases and advocating for TBI victims. In 2016, Tom Crosley achieved a record-breaking win in a widely publicized TBI case against the trampoline park company Cosmic Jump here in Texas.
If you or a loved one has suffered a brain injury due to someone else’s carelessness — especially if pituitary dysfunction resulted from the injury — call Crosley Law Firm at 210-LAW-3000 | 210-529-3000or fill out our free consultation request form.
We offer free consultations so we can listen to the details of your story and give you candid advice about what your best course of action is. We also handle personal injury claims on a contingent fee basis, which means you do not pay attorney fees or case expenses unless we get you a settlement or win your case in court. Don’t wait — contact us today!
References
Hacioglu A., Kelestimur F., Tanriverdi F. (2019, January). Pituitary dysfunction due to sports-related traumatic brain injury. Pituitary. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/30637622
Hypopituitary. (2016). WebMD. Retrieved from http://www.webmd.com/a-to-z-guides/hypopituitary#1
Tanriverdi, F., & Kelestimur, F. (2015). Pituitary dysfunction following traumatic brain injury: Clinical perspectives. Neuropsychiatric Disease and Treatment 11, pp. 1835-1843. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4524578/
TBI: Get the Facts. (2017, April 27). Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/traumaticbraininjury/get_the_facts.html
West, T. A., & Sharp, S. (2014, January). Neuroendocrine dysfunction following mild TBI: When to screen for it. The Journal of Family Practice 63(1), pp. 11-16. Retrieved from http://www.mdedge.com/jfponline/article/79596/pain/neuroendocrine-dysfunction-following-mild-tbi-when-screen-it
The content provided here is for informational purposes only and should not be construed as legal advice on any subject.